The hypothalamus in the brain releases GnRH (gonadotropin-releasing hormone) in a pulsatile fashion into the system every 60 to 90 minutes. In both sexes, this GnRH triggers the pituitary gland to release two additional hormones known as gonadotropins—FSH (follicle stimulating hormone) and LH (luteinizing hormone). During the reproductive years, this pulse activity is critical for successful reproductive function as controlled by feedback loops.
The FSH and LH that are released produce very different effects in the two sexes
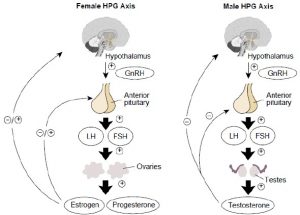
Hypothalamic–pituitary–gonadal axis
FSH and LH in a woman
In a woman, they stimulate the production of oestrogen and progesterone in the ovary. The release of these hormones in a woman’s system is cyclical. By this, we mean that GnRH received by a woman’s pituitary during the first half of the month stimulates predominantly the production of the FSH, which in turn stimulates the maturation and then—after an LH release—the release of an egg. But during the second half of the month, GnRH will cause a woman’s pituitary to produce predominantly the LH, which triggers the corpus luteum to produce progesterone and oestradiol to prepare the uterus for implantation.
FSH and LH in a man
Meanwhile, the release of FSH and LH into the male system is constant and chronic—in other words, both hormones are produced at an even rate throughout the month. The chronic release of both FSH and LH means that a man is fertile, or producing sperm cells, on a constant basis. If a woman’s pituitary released both FSH and LH at a constant rate, her reproductive system would lose its monthly rhythm and the time sequence to the ovulation-pregnancy or menstruation would be disrupted. Follicles and eggs would not grow and mature and the uterus would not develop a receptive lining. When compared to a woman’s cyclic pattern, the male system may sound simpler, but it is dependent on a perfect balance between FSH and LH being maintained at all times.
In a man, FSH and LH serve two entirely different purposes
FSH from the pituitary stimulates the Sertoli cells in the testicles to make viable sperm and spermatic fluid. It is critical for fertility and the lack of this hormone is by far the most common reason for male infertility (low sperm count) among male patients.
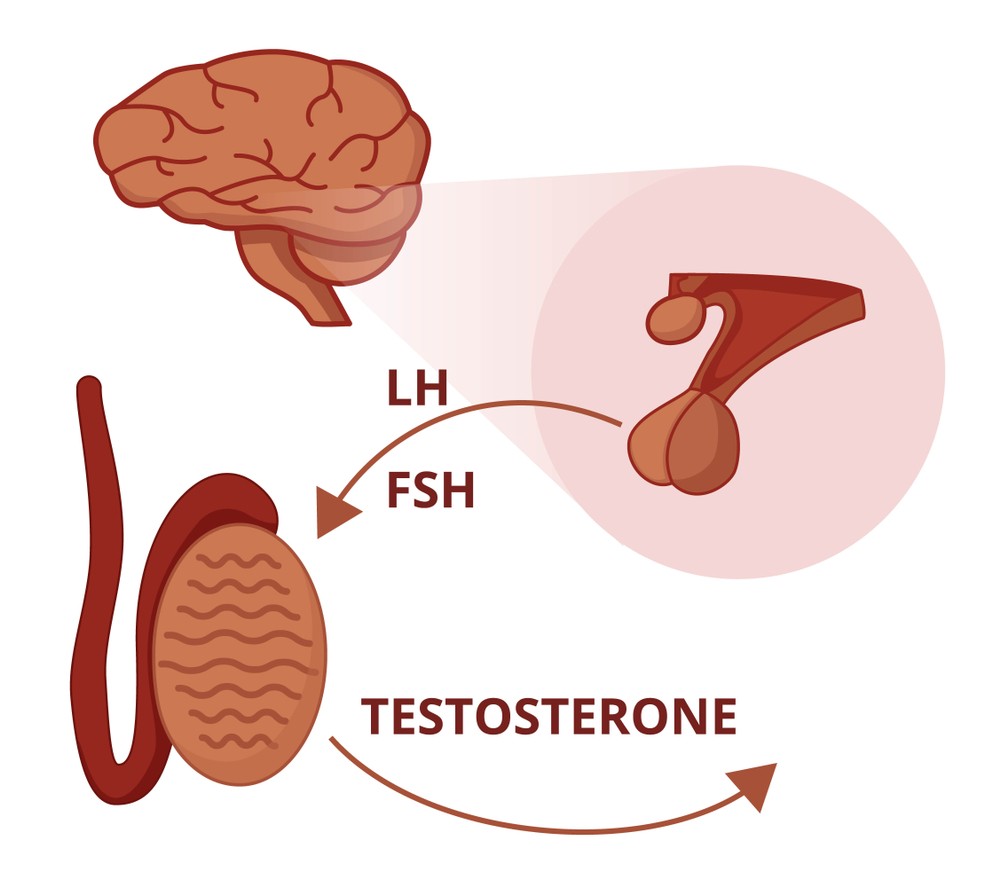
LH stimulates the Leydig cells in the testicles to make testosterone, the primary male hormone. When LH is affected, the production of testosterone is disrupted and a condition similar to having the testicles removed completely can occur and male sexual characteristics can be affected. Lack of this hormone is the main reason for hypogonadism (low testosterone).
This Hypothalamus-Pituitary-Gonad axis is maintained as a negative feedback loop that exogenous testosterone replacement (supplementation through pills, cream, patch, injection) can affect, potentially dampening FSH and LH production and this can have grave effects on male fertility.
My man is so masculine and he doesn’t produce sperm!
It is possible for either LH or FSH alone to cause the problems, while the other is normal. For example, if only the release of FSH is deficient, a man can have an infertility problem, yet not have any change in sexual characteristics, continuing to have normal ejaculatory function, beard growth, body shape, or sex drive. He will still be fully ‘male.’ The truth is, a man’s ability to reproduce rarely has any relation to the traits we commonly think of as ‘masculine.’