PCOS Facts:
|
In 1990s when I first qualified, PCOS was a rarity amongst my patients. Now it is commonplace and is estimated to affect close to one in five women.
Increased rates of PCOS are particularly common in populations that are undergoing lifestyle transition or “Westernisation”. This suggests that the syndrome is a result of entering into an evolutionarily novel environment, with the conflict between the modern environment and our ancient genome.
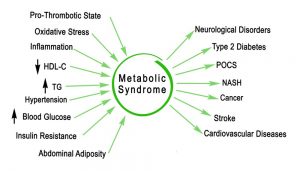
Metabolic disarray and its effects on gynaecology
Evidence shows that polycystic ovarian syndrome should not be seen purely as a gynaecological disorder but as a manifestation of a systemic metabolic condition.
PCOS and Insulin Resistance
It is well known that PCOS is intimately connected to insulin resistance. Insulin resistance and compensatory insulin excess (hyperinsulinemia) are one and the same disease. Insulin, as a nutrient sensor, encourages the growth of cells. In females of reproductive age, the most rapidly growing cells are the ovaries, so the hormonal environment is encouraging the excessive growth of these cysts in the ovaries.
Insulin: The Key Driver for Infertility
A high Insulin level appears to have an effect both on the brain by increasing luteinizing hormone (LH) levels, and directly on the ovary. Excess insulin sits on receptors on the theca cells, the outer coat of the ovary, and makes them more responsive to the hormonal environment, and therefore increases androgen (testosterone) production responsible for many of the clinical effects of PCOS. In addition, insulin decreases Sex Hormone Binding Globulin (SHBG) which increases the amount of free testosterone in the blood thus increasing the masculinising symptoms (hair growth etc.) seen in PCOS.
The higher LH and the higher androgen levels set up a signal that inhibits the follicle from ovulating. Each follicle grows and creates a lake of fluid around it but if it fails to burst and release its egg, a cyst is left. A situation then arises with a combination of high or normal oestrogen levels, high androgens, and low progesterone. This condition is usually characterized by obesity, especially middle-of-the-body obesity, androgen signs such as acne, oily skin, facial and breast hair and head hair loss. Since oestrogen levels tend to be higher with weight gain, these women have a greater risk of breast cancer and endometrial cancer. They may also have the worst PMS symptoms.
PCOS is notorious for misdiagnosis. It may take several years for patients to be correctly diagnosed. Beware of diagnosis by ultrasound alone because, since the ovaries change every month.
If you truly have PCOS, your blood tests will show at least one of the following:
- High androgens (testosterone or androstenedione or DHEA)
- Low SHBG
- High LH (luteinizing hormone)
Treatment strategy: PCOS is not a single disease
PCOS is a multifactorial disease that has significant clinical implications for reproductive, metabolic and psychological health and requires an individualized approach to treatment.
Herbal formulas are tailored to target the patient’s unique combination of symptoms rather than only treating the diagnosed condition.
We aim to:
- up-regulate insulin receptors and stimulates the uptake of glucose into cells.
- lower insulin and lower inflammation
- lower testosterone, reduce Luteinizing hormone
- promote ovulation and progesterone
- assist in the reduction of weight (belly fat): If you are overweight, losing as little as 5 per cent of your total body weight has been shown to improve fertility in PCOS.
Dr Ryu’s articles on PCOS
Insulin Resistance: The critical piece of the puzzle
General considerations for weight loss
Early-onset Balding, the first sign of Insulin Resistance