For couples trying to conceive, fertility is often seen as a black box – either it works or it doesn’t. However, there are intricate biochemical factors and metabolic processes happening behind the scenes that can dramatically impact one’s ability to get pregnant. One of the most influential and underappreciated of these is obesity. While carrying extra body fat may not seem like an obvious barrier to fertility at first glance, the metabolic changes that accompany obesity can significantly impair a woman’s reproductive capacity.
In recent decades, rates of obesity and overweight have been on the rise globally. Excess body weight is associated with increased risks for many diseases, including type 2 diabetes, heart disease, and some cancers. But obesity also wreaks subtle havoc on the complex hormonal pathways that allow for ovulation, conception, and healthy pregnancy.
HPO axis disruption
One of the primary ways obesity hinders fertility is by disrupting the hypothalamic-pituitary-ovarian axis. By Artoria2e5 – Own work, CC BY 3.0, https://commons.wikimedia.org/w/index.php?curid=81460023
This refers to the intricate feedback loop between the hypothalamus in the brain, the pituitary gland, and the ovaries. The hypothalamus produces gonadotropin-releasing hormone (GnRH), which triggers the pituitary gland to release follicle stimulating hormone (FSH) and luteinizing hormone (LH). These hormones then act on the ovaries to stimulate egg maturation and ovulation. But in obese women, high levels of body fat can impair the secretion of GnRH, leading to reduced FSH and LH release. This can cause irregular menstrual cycles, anovulation (lack of ovulation), and infertility.
Insulin resistance and PCOS
Obesity also promotes hormonal imbalances like those seen in polycystic ovary syndrome (PCOS). PCOS is a common endocrine disorder and cause of female infertility, affecting up to 10% of women of reproductive age. It is characterized by high testosterone levels, ovarian cysts, irregular periods, and metabolic disturbances like insulin resistance. The origins of PCOS are not fully understood, but excess body weight is known to exacerbate hormone abnormalities and reproductive dysfunction for many affected women. Losing weight may be one of the most effective ways to regulate menstrual cycles and improve fertility outcomes in obese women with PCOS.
Adipokines from fat cells
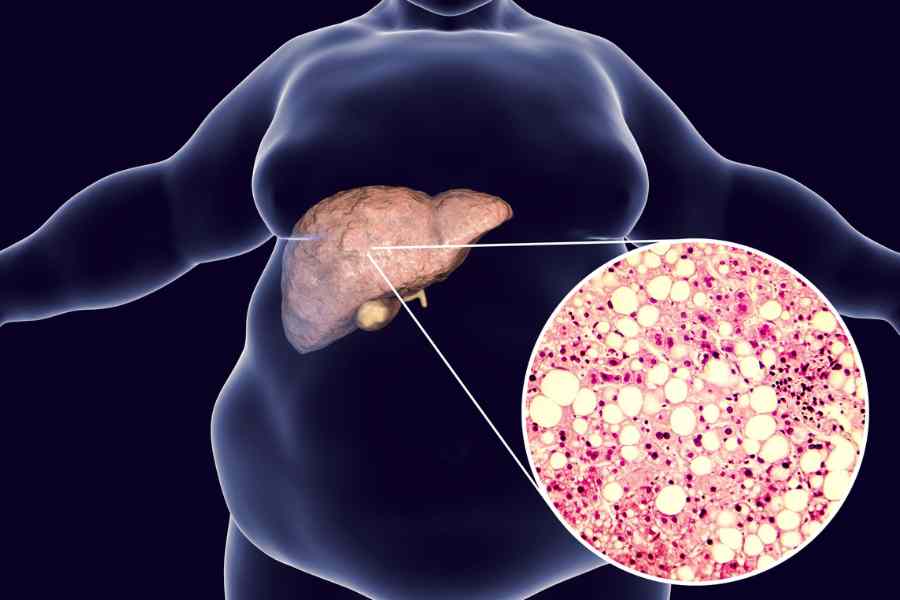
Additionally, fatty tissue is not inert – fat cells produce their own hormones and bioactive molecules called adipokines. Some of these adipokines, like leptin, directly impair ovulation. Adipokines can also contribute to systemic inflammation, insulin resistance, cardiovascular disease risk factors, and other issues that may compromise reproductive health. So in obese women, just having more fat cells pumping out metabolically-active signals can disrupt fertility through multiple avenues.
Egg quality concerns
Obesity also appears to directly affect the quality of a woman’s eggs. Within the ovaries, immature egg cells called oocytes must properly differentiate and mature to become viable for fertilization. But studies indicate the oocytes of obese women have impaired maturation, increased abnormalities, and reduced capacity to be fertilized.
Endometrial receptivity
Obesity also detrimentally affects endometrial receptivity – the ability of the uterus lining to accept and implant an embryo after fertilization.
Together, these obesity-related effects help explain why overweight and obese women tend to have lower conception rates and higher miscarriage rates than normal weight women. The intricacies of metabolism extend well beyond the scale, influencing reproduction on a biochemical level.
Metabolic health – the missing link
The good news is that losing weight, even just 5-10% of body weight, can rapidly improve many of these metabolic and hormonal abnormalities. Shedding visceral fat around the tummy area and achieving healthy body composition restore regular menstrual cycles, ovulation, and fertility in obese women. This is the reason we are serious about weight loss for fertility and hormonal health. For those struggling with infertility, optimizing body composition and metabolic health should be a priority before considering invasive and expensive fertility treatments.