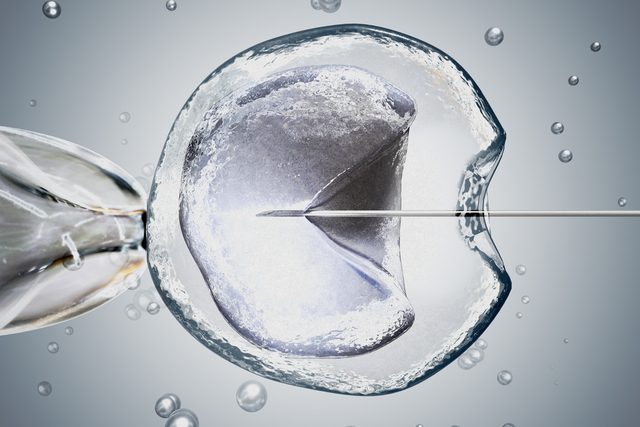
Since the birth of the first baby conceived through in vitro fertilization in 1978, the evaluation and treatment of the patient with infertility have undergone significant change and has influenced the medical practice dramatically.
Interest in identifying the underlying causes of the infertility problem has diminished significantly and the trend in the treatment of infertility has been in the development of various means to artificially replace the natural procreative system. A highly-technological approach to treating reproductive abnormalities is now replacing the previous treatments which were effective and affordable and often led to pregnancy.
IVF was originally invented to bypass tubal disease. The demand for IVF is unlikely to diminish given the delay in childbearing age and the high rates of chlamydial infection causing tubal disease. It is also notable that, although IVF was invented to bypass tubal disease, IVF success rates are lowest for that indication particularly in the presence of hydrosalpinges and it is now disputable if IVF is more successful than tubal surgery. While tubal disease accounts for only 25–35% of infertility in women, IVF is now suggested to treat (or bypass) a wide variety of fertility problems.
- Endometriosis? IVF
- PCOS? IVF
- Ageing ovaries? IVF
- Male factor infertility? IVF
- Unexplained infertility? IVF
- and even recurrent miscarriage? IVF.
Many programmes have developed protocols for the implementation of treatments for the infertile patient. This sequence almost invariably points to IVF.
|
It is recommended that for women over 35 years, the first two steps should be rapidly completed. For women under 30 years of age, more time can be spent on these steps.
It is notable that success rates for intrauterine insemination (IUI) are very similar to that for normal intercourse.
Real progress or perceived progress
Whilst the public is led to think that this is really the only viable approach available for their problem, one must begin to realistically question whether or not any real progress has been made in fertility field.
- On a “per-woman basis,” looking at endometriosis management, the pregnancy rates were higher two decades ago with the standard conservative surgery than they are currently with ART.
- In 1978, an intrauterine pregnancy rate of 29 percent could be expected in patients who underwent microsurgical salpingostomy (surgically correcting the tubal obstruction) while the National Summary for IVF reported a pregnancy rate per cycle started of 29.1 per cent for patients with tubal factor infertility
- Has there been fifty years of “progress” in pregnancy rates in patients with polycystic ovarian disease? In reality in 1950, the pregnancy rate from wedge resection was 66 per cent. In 2001, the pregnancy rate per cycle started with IVF was 23.1 percent.
Diagnosis and treatment over hyperstimulation and embryo transfer
Infertility in women can be caused by a multitude of factors including tubal factor, tubal/peritoneal factor, ovulatory dysfunction, endometriosis, diminished ovarian reserve, uterine/cervical factors, immunological factors, and unexplained reasons. Cervical mucus defects and disorders are infrequent causes of infertility (three per cent) and are difficult to diagnose with certainty. Male infertility plays an equal part in problems with conception and pregnancy maintenance although it is often overlooked and researched much less. Egg, sperm, embryo quality concerns are not addressed by IVF.
The causes of infertility are multi-factorial and very complex – much more so than is generally recognised. Yet IVF is seen to be the standard fertility treatment and bypass many of the underlying causes of infertility. Establishing a diagnosis before treatment and using a specific, often cheaper, treatment is often more satisfactory and restore fertility.